Abstract
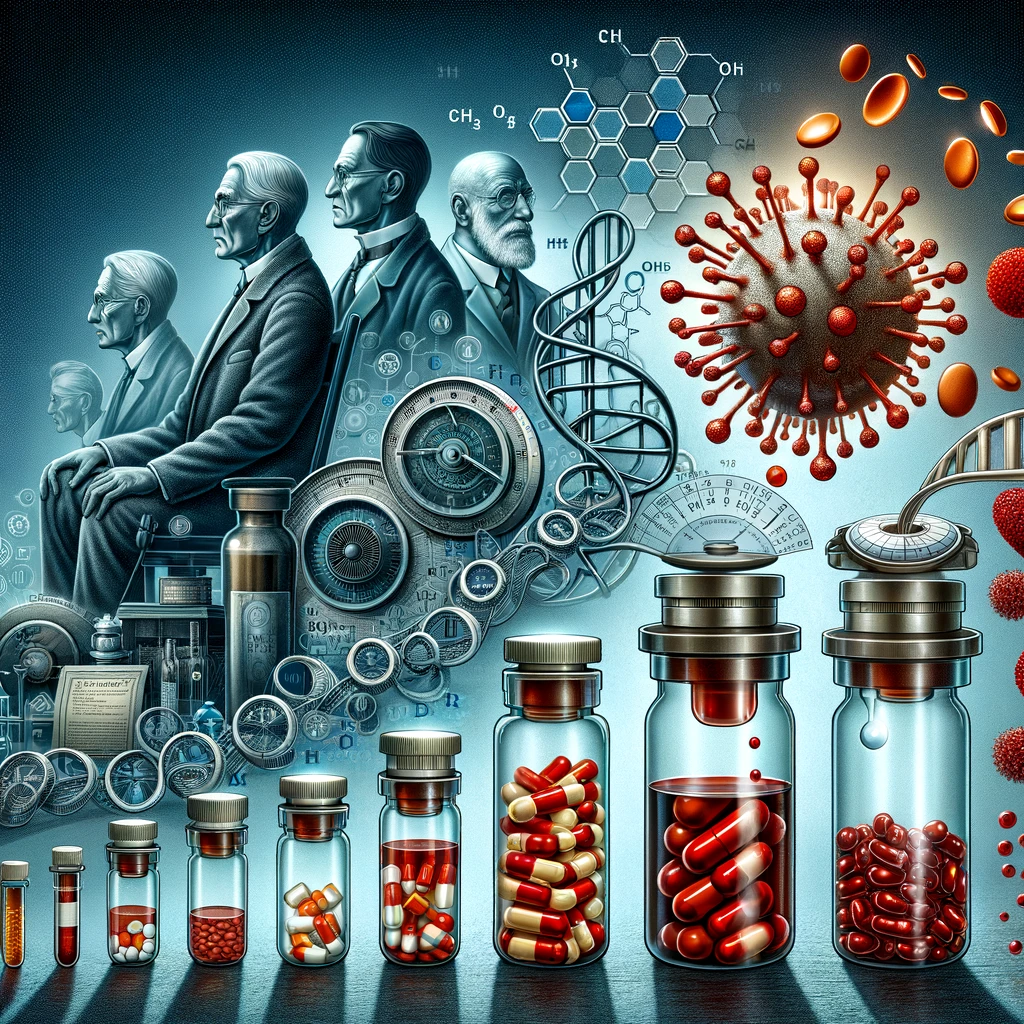
The advent of Direct Oral Anticoagulants (DOACs) has revolutionized the management of thromboembolic disorders, presenting a significant paradigm shift from traditional Vitamin K Antagonists (VKAs), such as warfarin. Introduced into clinical practice in 2008 with the approval of Dabigatran by the U.S. Food and Drug Administration (FDA), DOACs have expanded the therapeutic arsenal, offering distinct advantages in terms of efficacy, safety, and patient convenience. This article explores the development, mechanism of action, clinical applications, and comparative effectiveness of DOACs, underpinned by empirical data and clinical trials. Our objective is to provide a comprehensive overview for healthcare professionals navigating the complexities of anticoagulation therapy in a diverse patient population.
Introduction
Thromboembolic disorders represent a major cause of morbidity and mortality worldwide, necessitating effective anticoagulation strategies. The introduction of DOACs has provided clinicians with potent alternatives to VKAs. Unlike VKAs, which indirectly inhibit the synthesis of coagulation factors, DOACs directly target key enzymes in the coagulation cascade, namely Factor Xa and thrombin, offering a more predictable pharmacokinetic profile without the need for routine monitoring.
Development and Mechanism of Action
DOACs are classified into two main categories based on their mechanism of action: Factor Xa inhibitors (Rivaroxaban, Apixaban, and Edoxaban) and direct thrombin inhibitors (Dabigatran). Factor Xa inhibitors block the activity of Factor Xa, reducing the conversion of prothrombin to thrombin. Dabigatran, on the other hand, directly inhibits thrombin, preventing the conversion of fibrinogen to fibrin. This targeted approach not only enhances the specificity of anticoagulation therapy but also reduces the risk of bleeding complications associated with nonspecific inhibition of the coagulation cascade.
Clinical Applications and Efficacy
DOACs have been approved for various indications, including the prevention of stroke and systemic embolism in patients with non-valvular atrial fibrillation, the treatment and secondary prevention of venous thromboembolism (VTE), and the prevention of deep vein thrombosis (DVT) in patients undergoing hip or knee replacement surgery. Comparative studies and meta-analyses have demonstrated that DOACs are either comparable or superior to warfarin in reducing the risk of stroke and systemic embolism in patients with non-valvular atrial fibrillation, with a similar or reduced risk of major bleeding. For the treatment of VTE, DOACs have shown non-inferiority to conventional therapy with a favorable safety profile.
Advantages Over Traditional Anticoagulants
The primary advantages of DOACs over VKAs include a rapid onset of action, a predictable dose-response relationship, fewer food and drug interactions, and the elimination of routine coagulation monitoring. These attributes translate into improved patient adherence and satisfaction. However, considerations such as renal function, patient weight, and potential drug-drug interactions must guide the choice and dosing of DOACs to optimize therapeutic outcomes.
Conclusion
The introduction of DOACs represents a milestone in anticoagulation therapy, offering a balance of efficacy, safety, and convenience that challenges the longstanding dominance of VKAs. As our understanding of these agents continues to evolve, so too will their role in clinical practice, potentially extending to new indications and patient populations. Healthcare professionals must remain abreast of the latest evidence and guidelines to harness the full potential of DOACs in the management of thromboembolic disorders.
Author: David Halenta
Note: Before relying on the information in this article, please ensure you have read our Disclaimer for important legal and health information.
References
Eriksson, B.I., et al. (2008). “Dabigatran versus warfarin in the treatment of acute venous thromboembolism.” New England Journal of Medicine, 361(24), 2342-2352.
Patel, M.R., et al. (2011). “Rivaroxaban versus warfarin in nonvalvular atrial fibrillation.” New England Journal of Medicine, 365(10), 883-891.
Granger, C.B., et al. (2011). “Apixaban versus warfarin in patients with atrial fibrillation.” New England Journal of Medicine, 365(11), 981-992.
Cohen, A.T., et al. (2013). “Rivaroxaban for thromboprophylaxis in acutely ill medical patients.” New England Journal of Medicine, 368(6), 513-523.
Leave a Reply