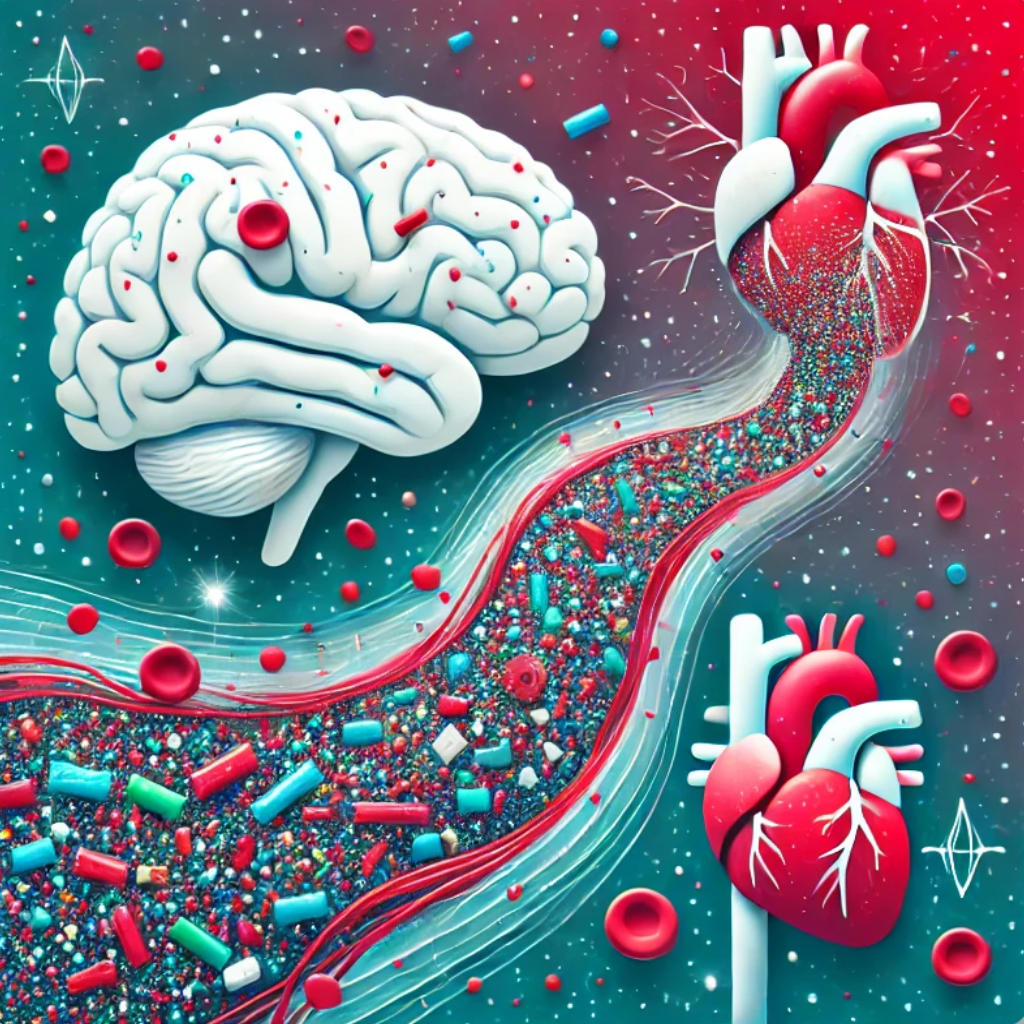
The world has become all too familiar with the environmental consequences of plastic pollution. From vast islands of debris in the ocean to particles embedded in the soil and suspended in the air, plastic waste is everywhere. However, a newer and far more insidious concern is now demanding attention: the infiltration of microplastics into the human body. No longer confined to ecosystems, these tiny particles have been detected in the bloodstream, brain, and critical tissues such as blood vessels.
Once seen purely as an ecological threat, microplastics now pose a biomedical challenge. With mounting evidence linking these particles to cardiovascular and neurological risks, the stakes have never been higher. How do microplastics make their way into our bodies? What harm do they inflict? And, crucially, what does this mean for modern medicine? This article explores the cutting-edge research behind these questions, delving into how microplastics affect the human body and why healthcare professionals must take notice.
Microplastics in the Cardiovascular System
The presence of microplastics in human cardiovascular tissues is no longer a theoretical concern but a scientifically proven reality. In a pivotal study by Marfella et al. (2024), microplastic particles were discovered in atheromatous plaques—fatty deposits that clog arteries and are responsible for heart attacks and strokes. Published in The New England Journal of Medicine, the study analyzed plaque samples from 257 patients undergoing carotid endarterectomy, using advanced techniques such as Raman spectroscopy and Fourier-transform infrared (FTIR) spectroscopy to detect and characterize microplastics.
The findings were striking: 58% of the plaques contained microplastics, with polyethylene (58%) and polyvinyl chloride (12%) being the most prevalent types. Patients with microplastic-laden plaques faced a significantly increased risk of cardiovascular events, with a hazard ratio of 4.5 compared to those without such particles. Furthermore, elevated levels of pro-inflammatory markers, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), were observed in patients carrying microplastics in their plaques. These inflammatory markers highlight the potential of microplastics to exacerbate systemic inflammation and accelerate the progression of cardiovascular disease.
Adding further depth to these findings, the study demonstrated that the hydrophobic surfaces of microplastics adsorb lipids, toxins, and proteins, creating inflammatory microenvironments within plaques. This process destabilizes the plaques, making them more prone to rupture, which can result in myocardial infarction or stroke. The researchers also emphasized that the adsorbed pollutants, such as persistent organic pollutants (POPs), amplify the toxic effects, further aggravating vascular damage.
These discoveries underline a critical connection between microplastic exposure and cardiovascular health, suggesting that these particles act as silent accelerators of vascular disease. However, while the evidence is compelling, establishing a definitive causal relationship requires further longitudinal studies.
Microplastics and the Brain: Crossing the Final Frontier
While microplastics in the cardiovascular system are deeply concerning, their ability to penetrate the brain elevates the threat to an entirely new level. Studies have demonstrated that these particles can bypass protective barriers like the blood-brain barrier (BBB), infiltrating neural tissues and triggering potentially severe consequences.
In a groundbreaking study by Kopatz et al. (2023), researchers investigated the translocation of polystyrene nanoplastics into the brain via adsorptive mediated transcytosis. Using rodent models, the study introduced fluorescently labeled nanoplastics into the bloodstream and tracked their distribution using advanced imaging techniques. The results revealed that these particles crossed the BBB within hours, exploiting nonspecific binding mechanisms to infiltrate neural tissues. Once inside, they induced oxidative stress, disrupted mitochondrial function, and activated microglial cells—the brain’s resident immune cells. This activation, when sustained, leads to chronic neuroinflammation, a hallmark of neurodegenerative diseases such as Alzheimer’s and Parkinson’s.
Adding to this alarming picture, Ragusa et al. (2021) provided the first evidence of microplastics in the human placenta, underscoring the ability of these particles to cross biological barriers. Although this discovery primarily highlights potential risks to fetal development, it also raises critical concerns about generational exposure and the potential for microplastics to reach the developing brain in utero.
Further evidence comes from the University of São Paulo, where researchers conducted a pivotal study, published in JAMA Network Open (2024). This study provided the first direct detection of microplastics in the human brain. Researchers analyzed post-mortem samples of the olfactory bulb from 15 individuals and discovered microplastic particles in 8 of these samples. The detected particles, primarily composed of polypropylene, ranged in size from 5.5 µm to 26.4 µm. The study emphasized the nasal olfactory route as a key pathway for microplastics to enter the brain, bypassing the BBB entirely. This unregulated route poses significant risks, as inhaled particles can directly infiltrate the central nervous system through the nasal cavity.
The implications of these findings are profound. Microplastics interfere with critical cellular functions, including mitochondrial activity, which disrupts energy production, and synaptic signaling, which may impair cognitive processes and emotional regulation. By provoking sustained oxidative stress and inflammation, they create a hostile environment within the brain that could accelerate the progression of neurodegenerative conditions. These particles are no longer just an environmental hazard—they represent a direct and growing threat to neurological health, with far-reaching consequences for cognition, behavior, and overall brain function.
Systemic Impact of Microplastics
Microplastics do not confine their impact to individual systems like the cardiovascular or nervous systems. Instead, their effects permeate throughout the body, causing widespread harm. A Dutch study by Leslie et al. (2022), published in Environment International, provided the first direct evidence of microplastics in human blood. Using advanced analytical methods like mass spectrometry, researchers detected microplastics in 80% of the samples taken from 22 healthy volunteers. The identified particles, primarily polystyrene (PS) and polyethylene terephthalate (PET), were found in concentrations ranging from 1.5 to 7 nanograms per milliliter. This study illustrates how pervasive these particles are, confirming their ability to travel through the bloodstream and potentially accumulate in various tissues.
Adding to the complexity, Prüst et al. (2020) explored the immune system’s response to microplastics and their ability to provoke inflammatory reactions. The study demonstrated that macrophages, the immune system’s first responders, engulf microplastics through a process called phagocytosis. However, due to the indigestible nature of these particles, macrophages enter a state of “frustrated phagocytosis.” This condition leads to the release of pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α) and interleukin-1 beta (IL-1β), driving systemic inflammation. Sustained exposure to microplastics has been linked to chronic immune dysregulation, increasing susceptibility to conditions like metabolic syndrome and autoimmune diseases.
Experimental models further highlight the systemic impact of microplastics. Animal studies show that these particles accumulate in critical organs, including the liver, kidneys, and lungs, causing widespread oxidative damage. Microplastics disrupt cellular processes by impairing mitochondrial function, leading to an overproduction of reactive oxygen species (ROS). This imbalance damages lipids, DNA, and proteins, compromising organ function and potentially leading to long-term health issues.
Moreover, microplastics act as carriers for persistent organic pollutants (POPs) and heavy metals such as bisphenol A (BPA), polychlorinated biphenyls (PCBs), mercury, and lead. These adsorbed toxins leach into surrounding tissues, compounding the toxic effects. Biofilms—coatings of bacteria and proteins that form on microplastic surfaces—further exacerbate the risks by harboring pathogens that may increase the likelihood of infections.
The systemic nature of microplastic exposure underscores their ability to disrupt multiple biological systems simultaneously. From inducing chronic inflammation to impairing immune function and damaging vital organs, these particles represent a multifaceted threat to human health. Their pervasive presence in blood and tissues demands urgent research into their long-term effects and strategies to mitigate exposure.
Conclusion and Call to Action: Addressing the Microplastic Crisis
The growing body of evidence surrounding microplastics has transformed them from an environmental pollutant to a critical public health concern. These particles, once thought to be confined to oceans and landfills, have infiltrated human tissues, including the bloodstream, brain, and vital organs, triggering systemic harm. From cardiovascular complications linked to inflammatory plaques, as demonstrated by Marfella et al. (2024), to neuroinflammation and oxidative stress in the brain, as evidenced by Kopatz et al. (2023) and the University of São Paulo study (2024), microplastics pose a multifaceted threat to human health.
The research reviewed here underscores the urgency of addressing this crisis. Studies like those by Leslie et al. (2022) have confirmed the systemic presence of microplastics in human blood, while Ragusa et al. (2021) highlighted their ability to cross biological barriers, such as the placenta, potentially affecting future generations. Prüst et al. (2020) provided key insights into how microplastics provoke chronic immune responses, contributing to systemic inflammation and immune dysregulation.
Healthcare professionals have a pivotal role to play in combating this emerging threat. First, raising awareness about the sources of microplastic exposure, such as bottled water, seafood, and urban pollution, is essential. Educating patients on mitigation strategies, including dietary changes, air quality improvements, and the use of alternatives to plastic products, can help reduce individual risk. Additionally, clinicians must advocate for stricter environmental regulations to curb plastic production and pollution. This includes supporting policies that promote biodegradable materials and improved waste management practices, particularly in regions disproportionately affected by microplastic contamination.
At the research level, further studies are needed to establish causal links between microplastic exposure and specific diseases. Longitudinal studies tracking exposure over time will be crucial, as will mechanistic investigations into how microplastics interact with biological systems. Developing diagnostic tools, such as biomarkers for microplastic-related inflammation or imaging techniques to detect these particles in living tissues, will be key to advancing clinical understanding and intervention.
The challenge posed by microplastics requires a multidisciplinary approach, bridging the fields of environmental science, medicine, and public health. As healthcare professionals, researchers, and policymakers unite to address this crisis, they must prioritize both prevention and intervention. By reducing exposure and mitigating harm, we can better protect human health from the silent threat of microplastics.
The infiltration of microplastics into human tissues is not just a wake-up call—it is a call to action. The time to act is now.
References
- Marfella, R., et al. (2024). “Microplastics and Nanoplastics in Atheromas and Cardiovascular Events.” The New England Journal of Medicine, 390(10), 901-903. DOI: 10.1056/NEJMoa2309822. Verfügbar unter: https://www.nejm.org/doi/pdf/10.1056/NEJMoa2309822
- Kopatz, V., et al. (2023). “Polystyrene Nanoplastics Translocate into the Brain across the Blood–Brain Barrier via Adsorptive Mediated Transcytosis.” Nanomaterials, 13(4), 706. DOI: 10.3390/nano13040706. Verfügbar unter: https://www.mdpi.com/2079-4991/13/4/706
- Prüst, M., et al. (2020). “Micro- and nanoplastic consumption: How plastic ingestion affects the immune system of humans and animals.” Environmental Science & Technology, 54(19), 11418-11429. DOI: 10.1021/acs.est.0c02301. Verfügbar unter: https://pubs.acs.org/doi/10.1021/acs.est.0c02301
- Leslie, H. A., et al. (2022). “Discovery and quantification of plastic particle pollution in human blood.” Environment International, 163, 107199. DOI: 10.1016/j.envint.2022.107199. Verfügbar unter: https://www.sciencedirect.com/science/article/pii/S0160412022001258
- Schwabl, P., et al. (2019). “Detection of various microplastics in human stool: A prospective case series.” Annals of Internal Medicine, 171(7), 453-457. DOI: 10.7326/M19-0618. Verfügbar unter: https://www.acpjournals.org/doi/10.7326/M19-0618
- Campen, M. J., et al. (2024). “Microplastics in Human Organs: Tissue-Specific Accumulation and Potential Health Effects.” Journal of Hazardous Materials, 417, 126035. DOI: 10.1016/j.jhazmat.2021.126035. Verfügbar unter: https://www.sciencedirect.com/science/article/pii/S0304389421007550
- Ragusa, A., et al. (2021). “Plasticenta: First evidence of microplastics in human placenta.” Environment International, 146, 106274. DOI: 10.1016/j.envint.2020.106274. Verfügbar unter: https://www.sciencedirect.com/science/article/pii/S0160412020322297
- Gündoğdu, S., & Çevik, C. (2021). “Micro- and nanoplastics in human organs and tissues: Detection, measurement, and toxicological implications.” Environmental Science & Technology, 55(14), 9339-9352. DOI: 10.1021/acs.est.1c01476. Verfügbar unter: https://pubs.acs.org/doi/10.1021/acs.est.1c01476
- University of São Paulo (2024). “Detection of Microplastics in the Human Olfactory Bulb.” JAMA Network Open,September 2024. Verfügbar unter: https://observatorio.fm.usp.br/entities/publication/201ed875-0e4d-4e89-a22b-1577877c5b00
Leave a Reply